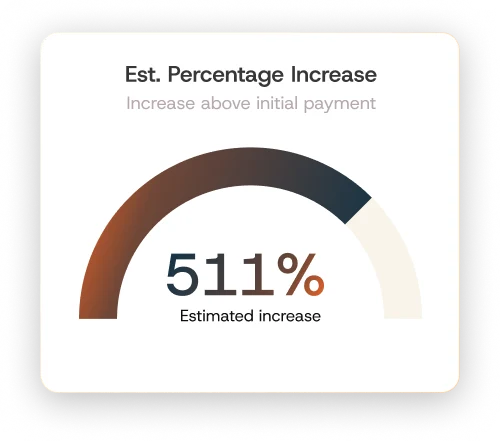
Identify the claims that matter, avoid the ones that don’t.
Providers face millions of claims and limited time to determine which ones are worth pursuing in IDR. Our eligibility engine surfaces high-value, often-missed claims that can add up to millions in uncaptured revenue, while also flagging the claims that shouldn’t be submitted.

- Finds complex, easily overlooked revenue opportunities
- Filters out ineligible and non-compliant claims
- Designed for providers and hospital systems of all sizes
- Learns from prior IDR determinations
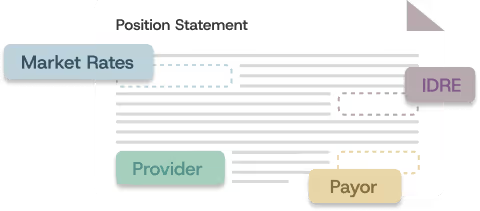
- Tailors arguments by payer, code set, and IDRE
- Generates clean, defensible, fully compliant statements
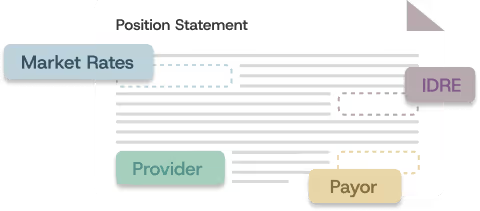
Custom Position Statements
Data-backed arguments that win claims.
Winning in IDR is rarely about a single factor. It’s about how claim details, payer behavior, IDRE workflows, and market data come together. Pivotal Health’s proprietary engine analyzes millions of data points to build precise, custom position statements designed to perform across a wide range of IDR scenarios.
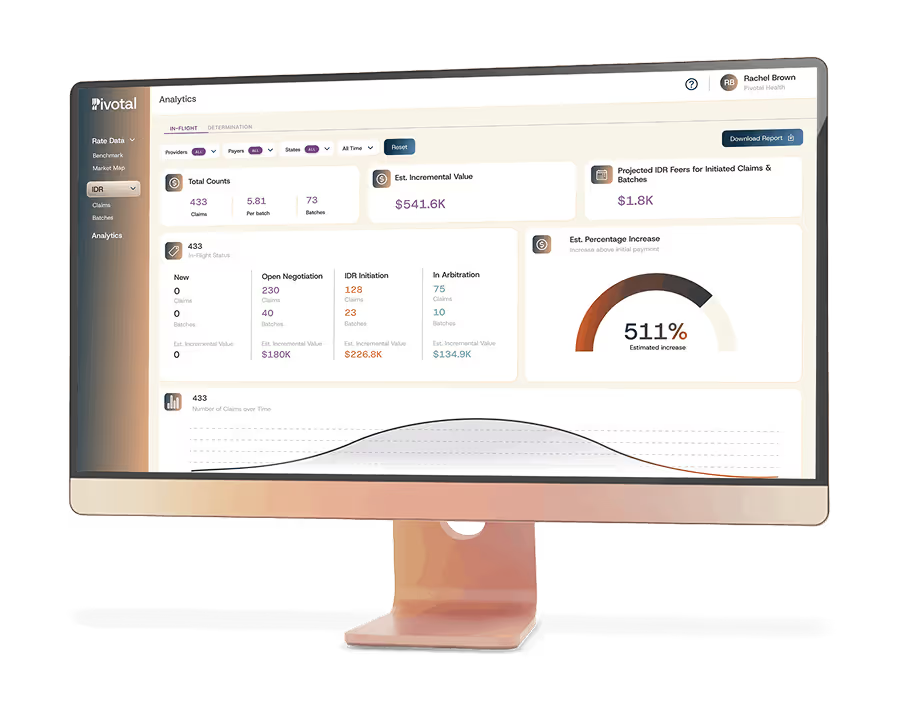
Intelligence Batching Technology
Reduce fees. Increase returns. Total visibility—no guesswork.
Batching can significantly reduce IDR costs, but only when it’s done correctly and transparently. Our batching engine automatically groups eligible claims according to federal and state rules, maximizing cost efficiency, ensuring compliance, and giving you full visibility into every decision we make.
- Lower IDR fees with smart, compliant batching
- Higher returns through optimized groupings
- Full visibility into every batching decision